Study Objectives
To determine the effects of sleep and sleep deprivation on plasma melatonin concentrations in humans and whether these effects are age-dependent.
Design
At least 2 weeks of regular at-home, sleep/wake schedule followed by 3 baseline days in the laboratory and at least one constant routine (sleep deprivation).
Setting
General Clinical Research Center (GCRC), Brigham and Women’s Hospital, Boston, MA.
Participants
In Study 1, one group (<10 lux when awake) of 19 young men (18-30 y) plus a second group (<2 lux when awake) of 15 young men (20-28 y) and 10 young women (19-27 y); in Study 2, 90 young men (18-30 y), 18 older women (65-81 y), and 11 older men (64-75 y). All participants were in good health, as determined by medical and psychological screening.
Interventions
One to three constant routines with interspersed inversion of the sleep/wake cycle in those with multiple constant routines.
Measurements and Results
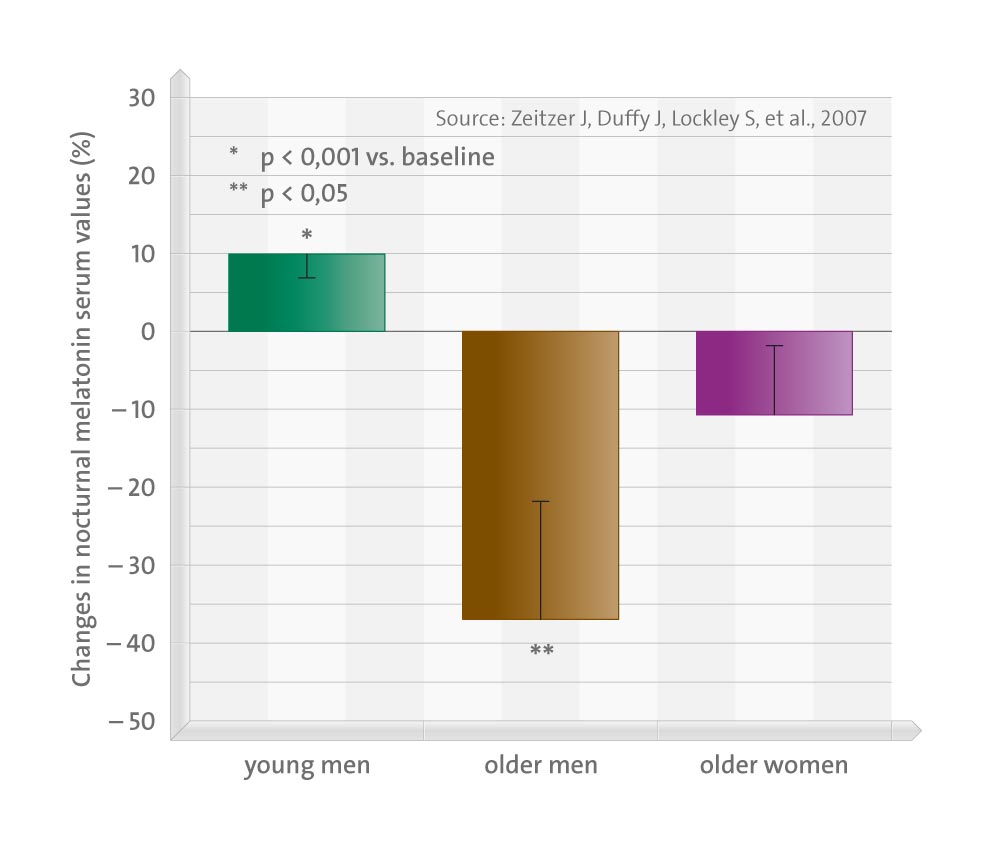
Examination of plasma melatonin concentrations and core body temperature. Study 1. There was a small, but significant effect of sleep deprivation of up to 50 hours on melatonin concentrations (increase of 9.81 +/- 3.73%, P <0.05, compared to normally timed melatonin). There was also an effect of circadian phase angle with the prior sleep episode, such that if melatonin onset occurred <8 hours after wake time, the amplitude was significantly lower (22.4% +/- 4.79%, P <0.001). Study 2. In comparing melatonin concentrations during sleep to the same hours during constant wakefulness, in young men, melatonin amplitude was 6.7% +/- 2.1% higher(P <0.001) during the sleep episode. In older men, melatonin amplitude was 37.0% +/- 12.5% lower (P <0.05) during the sleep episode and in older women, melatonin amplitude was non-significantly 10.9% +/- 8.38% lower (P = 0.13) during the sleep episode.
Conclusions
Both sleep and sleep deprivation likely influence melatonin amplitude, and the effect of sleep on melatonin appears to be age dependent.